Are you confused about the difference between obesity and morbid obesity? Understanding these terms can be crucial for your health and well-being.
While both involve excess body fat, morbid obesity is a more severe condition with greater risks and challenges. Knowing where you stand can help you take the right steps toward a healthier life. You’ll discover what sets obesity apart from morbid obesity, how each affects your body, and why it matters for your future.
Keep reading to learn how this knowledge can empower you to make better choices for your health.
Bmi And Classification
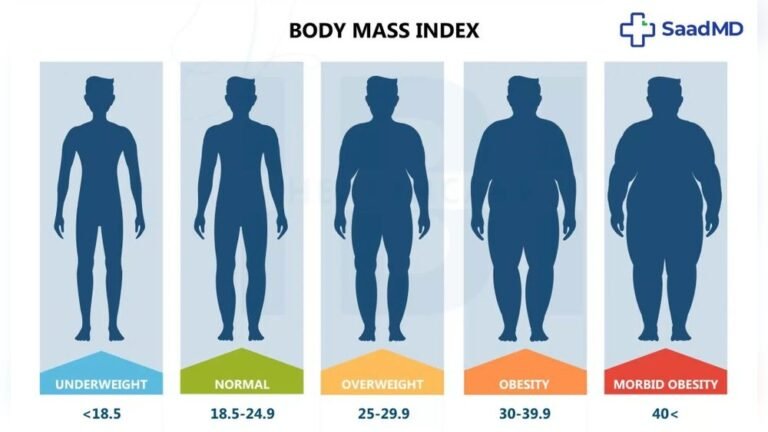
Body Mass Index (BMI) plays a key role in classifying obesity. It helps doctors identify the severity of excess body fat. This classification guides treatment and health risk assessment. Understanding BMI ranges clarifies the difference between obesity and morbid obesity.
Bmi Ranges For Obesity
BMI measures weight relative to height. A BMI of 30 to 34.9 is considered Class I obesity. Class II obesity includes BMIs from 35 to 39.9. These ranges indicate increased health risks but may be managed with lifestyle changes. BMI over 40 signals more serious obesity.
Class Iii Obesity Explained
Class III obesity, formerly called morbid obesity, starts at a BMI of 40 or higher. This level greatly raises the risk of severe health problems. It can affect mobility and strain organs like the heart and lungs. Often, this class requires intensive treatment such as surgery.
Limitations Of Bmi
BMI does not measure body fat directly. It cannot distinguish between muscle and fat mass. Athletes or muscular people may have a high BMI but low fat. BMI also ignores fat distribution, which affects health risks. Doctors use other tests alongside BMI for accurate assessment.

Credit: www.drlogy.com
Health Risks
Obesity and morbid obesity both carry serious health risks. These conditions affect the body in different ways. The level of risk increases as weight rises. Understanding these risks helps people make informed health choices.
Risks Linked To Obesity
Obesity raises the chance of many diseases. High blood pressure and type 2 diabetes are common problems. It also increases the risk of heart disease and stroke. Excess fat can lead to sleep apnea and joint pain. These issues reduce quality of life and can shorten lifespan.
Severe Risks In Morbid Obesity
Morbid obesity causes more severe health problems. The risk of heart failure and certain cancers grows higher. Breathing becomes difficult due to lung strain. Mobility often suffers, leading to muscle weakness. This stage demands stronger medical care and sometimes surgery.
Impact On Physical Function
Both obesity and morbid obesity reduce physical ability. Daily activities become harder, causing fatigue and pain. Morbid obesity often limits movement severely. This loss of function affects independence and mental health. Early action is key to preserving body function.
Symptoms And Physical Effects
The symptoms and physical effects of obesity and morbid obesity differ in intensity and impact. Both conditions involve excess body fat, but morbid obesity presents more severe health challenges. Understanding these differences helps recognize risks and the need for medical care.
Common Symptoms In Obesity
Obesity often shows through increased body weight and fat accumulation. People may feel tired more easily and notice shortness of breath during activity. There can be joint pain, especially in knees and hips. Skin issues like irritation and infections are common. High blood pressure and elevated blood sugar levels may start to appear.
Mobility Challenges In Morbid Obesity
Morbid obesity greatly limits movement and daily activities. Walking or standing for long periods becomes difficult. The extra weight puts intense pressure on bones and joints. Muscle weakness and fatigue are frequent. Some may use mobility aids or need assistance for basic tasks. Balance problems increase the risk of falls and injuries.
Other Physical Complications
Both conditions raise the chance of serious health problems. Morbid obesity increases risks for heart disease, stroke, and type 2 diabetes. Breathing difficulties such as sleep apnea are common. Digestive issues like acid reflux often occur. The immune system weakens, making infections more likely. Skin folds may develop sores and infections due to poor air circulation.

Credit: springfieldwellnesscentre.com
Causes And Contributors
The causes and contributors of obesity and morbid obesity overlap but vary in impact. Both conditions result from complex interactions of multiple factors. Understanding these factors helps in managing weight and reducing health risks.
Some causes trigger mild weight gain, while others lead to severe obesity. The difference often lies in lifestyle, genetics, and environment.
Lifestyle Factors
Diet plays a major role in weight gain. Consuming more calories than the body burns leads to fat storage. Sedentary behavior reduces calorie use, increasing risk. Poor sleep patterns can also disrupt metabolism. Stress may lead to overeating or unhealthy food choices. Together, these habits can cause or worsen obesity and morbid obesity.
Genetic Influences
Genes affect how the body stores fat and uses energy. Some people inherit a tendency to gain weight more easily. Genetics can influence appetite control and fat distribution. These inherited traits may increase the risk of severe obesity. Although genes matter, they work with lifestyle and environment to shape weight.
Environmental Triggers
Access to healthy food varies by location. Fast food and processed snacks are often cheaper and more available. Urban design may limit opportunities for physical activity. Social and cultural norms can affect eating habits. Exposure to certain chemicals might also impact metabolism. These triggers push weight gain beyond simple overeating.
Treatment Approaches
Treatment approaches for obesity and morbid obesity vary by severity and health risks. Both conditions require careful management to improve health and quality of life. Early intervention can prevent complications and reduce long-term damage.
Choosing the right treatment depends on individual needs, BMI level, and presence of other health issues. Doctors often combine different methods to achieve the best results.
Lifestyle Modifications
Lifestyle changes form the foundation of treatment for obesity. A balanced diet with controlled calories helps reduce weight safely. Regular physical activity boosts metabolism and supports heart health. Behavioral therapy teaches healthier habits and coping skills. Small changes, maintained over time, can lead to lasting weight loss.
For morbid obesity, lifestyle modifications alone may not be enough. Still, they remain essential alongside other treatments to maintain progress and improve well-being.
Medication Options
Doctors may prescribe medications to help control appetite or reduce fat absorption. These drugs support weight loss but require medical supervision. Medication suits patients with obesity who struggle to lose weight through lifestyle changes. It also helps some with morbid obesity before or after surgery.
Medications are not a quick fix. They work best combined with diet and exercise. Side effects and risks must be carefully considered by healthcare providers.
Surgical Interventions
Surgery is often recommended for morbid obesity or when other methods fail. Procedures like gastric bypass and sleeve gastrectomy reduce stomach size to limit food intake. Surgery can lead to significant, sustained weight loss and improve related health conditions.
Patients need lifelong medical follow-up after surgery. Surgery is not for everyone and requires careful evaluation by specialists. It offers hope for those facing severe health risks due to extreme obesity.
Terminology And Stigma
Understanding the terminology around obesity and morbid obesity is important. Words shape how society sees people with these conditions. Stigma can affect feelings and care quality. Clear, respectful language helps reduce bias and improves health outcomes.
Shifting Language: Morbid To Class Iii
The term “morbid obesity” sounds harsh and negative. Medical groups now prefer “Class III obesity” instead. This change focuses on health facts, not judgment. It helps patients feel less blamed for their weight. Using neutral terms encourages better conversations about treatment.
Social Perceptions
People often hold stereotypes about obesity and morbid obesity. These views can lead to unfair treatment and discrimination. Society sometimes sees obesity as a personal failure. This stigma can cause shame and isolation. Changing how we talk about these conditions can challenge these wrong ideas.
Impact On Patient Care
Stigma affects how patients seek medical help. Fear of judgment can delay doctor visits. Health professionals may unconsciously treat obese patients differently. Using respectful language improves trust between patients and doctors. Better communication leads to more effective care and support.

Credit: mexicobariatriccenter.com
Conclusion
Obesity and morbid obesity both affect health but differ in severity. Obesity often responds well to diet and exercise changes. Morbid obesity carries higher health risks and may need stronger treatments. Knowing your BMI helps understand these differences clearly. Early action can prevent serious complications later.
Always seek medical advice for proper care. Managing weight improves quality of life and reduces health problems. Small, steady steps make a big difference over time. Choose health every day for a better future.