Are you curious about how obesity and morbid obesity differ, especially when it comes to BMI? Understanding these differences is more than just knowing numbers—it’s about recognizing how your body’s weight impacts your health and what steps you can take to protect yourself.
Your BMI is a simple number, but it holds powerful information about your risk for serious health problems. You’ll discover exactly what sets obesity apart from morbid obesity based on BMI, why it matters to you, and how knowing this can guide you toward better health decisions.
Keep reading to gain clarity on these terms and take control of your well-being today.
Bmi And Weight Categories
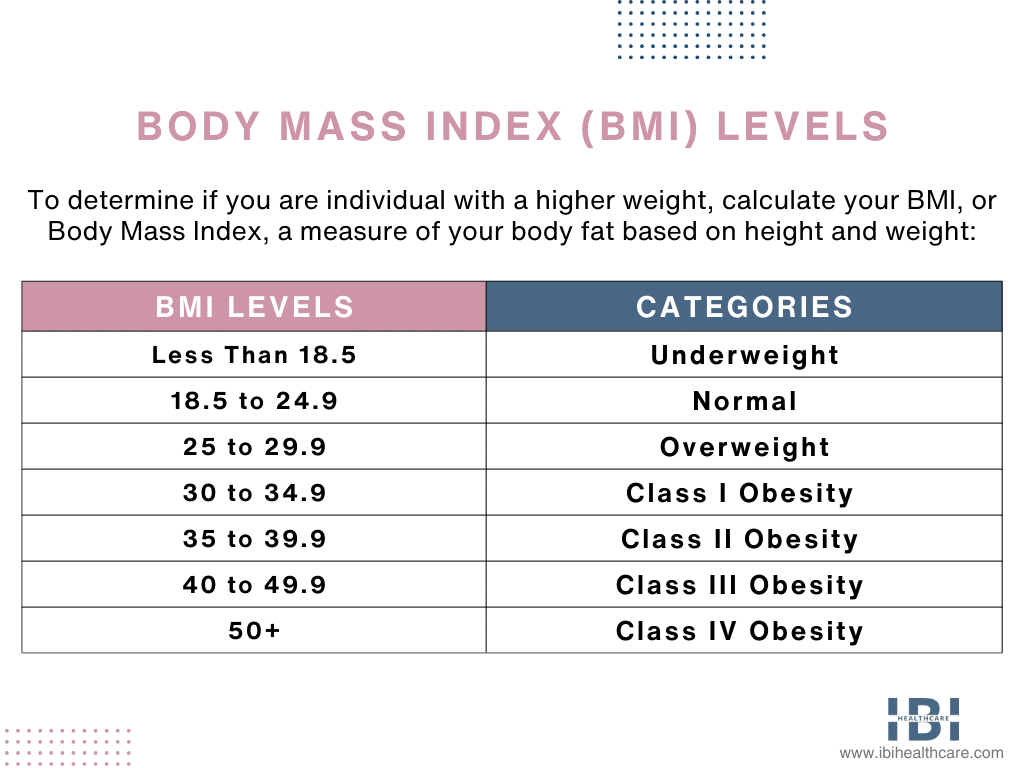
Body Mass Index (BMI) plays a key role in identifying weight categories. It helps classify weight status based on height and weight. Understanding BMI is essential to distinguish between obesity and morbid obesity. This section explains BMI calculation, ranges, and its limits.
Calculating Bmi
BMI is calculated by dividing weight in kilograms by height in meters squared. The formula is simple and widely used. This number gives a rough estimate of body fat. It allows quick screening of weight-related health risks.
Bmi Ranges Explained
BMI values fall into specific categories. A BMI under 18.5 means underweight. From 18.5 to 24.9 is normal weight. Overweight is 25 to 29.9, and obesity starts at 30. Morbid obesity, or Class III obesity, is a BMI of 40 or more. These ranges help doctors assess health risks linked to weight.
Limitations Of Bmi
BMI does not measure body fat directly. It ignores muscle mass, bone density, and fat distribution. Athletes may have high BMI but low fat. Older adults may have normal BMI but high fat. Other tools like waist circumference may give better insight into health.

Credit: www.drlogy.com
Obesity Classes
Obesity is divided into different classes based on Body Mass Index (BMI). These classes help doctors assess health risks linked to body weight. BMI measures body fat using height and weight. The higher the BMI, the greater the risk of health problems. Understanding these classes guides treatment and lifestyle changes.
Class I And Ii Obesity
Class I obesity means a BMI between 30 and 34.9. Class II obesity ranges from 35 to 39.9 BMI. People in these classes face increased risks of diabetes, heart disease, and high blood pressure. Lifestyle changes and medical support often help manage health risks.
Class Iii Obesity (morbid Obesity)
Class III obesity starts at a BMI of 40 or higher. It is also called morbid obesity. This class poses serious health risks like sleep apnea, severe heart issues, and joint problems. Medical treatments, including surgery, may be necessary to reduce these risks.
Super Morbid Obesity
Super morbid obesity refers to a BMI of 50 or more. It is an extreme form of obesity with very high health dangers. People in this category often require intensive medical care. Managing super morbid obesity usually involves a team of healthcare professionals.
Health Risks Linked To Obesity
Obesity affects millions worldwide and brings serious health risks. It increases the chance of many diseases and lowers life quality. Understanding these risks helps in managing health better. The dangers grow as weight rises, especially in morbid obesity. This section explains the health issues linked to obesity, highlighting common problems and those worsened by morbid obesity.
Common Complications
Obesity often leads to high blood pressure and type 2 diabetes. It raises the risk of heart disease and stroke. Breathing problems like sleep apnea are common. Fatty liver disease and certain cancers also appear more often. These conditions reduce life expectancy and increase medical costs.
Risks Amplified By Morbid Obesity
Morbid obesity greatly increases health dangers. The risk of heart failure and severe diabetes complications grows. Liver problems may become life-threatening. Mental health issues like depression are more frequent. Surgery risks rise due to extra strain on the body.
Impact On Joint And Mobility
Extra weight puts pressure on joints, causing pain. Knee and hip problems limit movement and daily tasks. Osteoarthritis develops faster in obese individuals. Walking and standing become difficult with morbid obesity. Loss of mobility affects independence and quality of life.
Symptoms And Signs
Recognizing the symptoms and signs of obesity and morbid obesity is vital. These indicators differ in severity but signal health risks. Early awareness helps in seeking proper care and support.
Physical Indicators
Obesity often shows as excess body fat and weight gain. Morbid obesity is more severe, with BMI over 40. Physical signs include difficulty moving, shortness of breath, and joint pain. Skin may develop stretch marks and folds. High blood pressure and sleep apnea are common in morbid obesity.
Psychological Effects
Both conditions can impact mental health. Feelings of low self-esteem and body shame often appear. Anxiety and depression may develop due to social stigma. Morbid obesity can cause stronger emotional distress and isolation. Support from healthcare providers is crucial to manage these effects.
Quality Of Life Concerns
Obesity limits daily activities and energy levels. Morbid obesity worsens these problems significantly. Simple tasks like walking or climbing stairs become hard. Sleep disturbances and fatigue reduce overall well-being. Health complications also affect work and social life.
Causes And Contributing Factors
The causes and contributing factors of obesity and morbid obesity are complex. Many elements work together to affect body weight. Understanding these factors helps in prevention and treatment.
Both obesity and morbid obesity share similar causes but differ in severity and impact. These causes include genetics, lifestyle, diet, and environmental influences.
Genetic Influences
Genes can affect how the body stores fat and uses energy. Some people inherit a tendency to gain weight easily. Genetic factors also influence appetite and metabolism rates. This makes some individuals more prone to obesity and morbid obesity.
Lifestyle And Diet
Poor eating habits contribute heavily to weight gain. Diets high in sugar, fat, and processed foods increase obesity risk. Sedentary lifestyles with little physical activity worsen this risk. Over time, these habits lead to excess body fat and higher BMI.
Environmental Factors
The surroundings where people live affect their weight. Easy access to unhealthy foods promotes overeating. Lack of safe spaces for exercise limits physical activity. Stress and lack of sleep also play roles in weight gain. These factors can push someone from obesity to morbid obesity.
Credit: www.ibihealthcare.com
Treatment Approaches
Treatment approaches for obesity and morbid obesity differ due to varying health risks. Both conditions require careful management to improve quality of life. Selecting the right treatment depends on the body mass index (BMI) and overall health status. Below are the main treatment paths explored by medical professionals.
Diet And Exercise
Diet changes form the foundation of weight management. Patients learn to reduce calorie intake with balanced meals. Exercise helps burn calories and strengthens the heart and muscles. For morbid obesity, physical activity may start slow and increase gradually. Consistency in diet and exercise can prevent further weight gain.
Medical Interventions
Doctors may prescribe medication to support weight loss. These drugs reduce appetite or block fat absorption. Medical treatment suits those who cannot lose weight by diet and exercise alone. Regular monitoring ensures medication safety and effectiveness. Medical interventions often accompany lifestyle changes for best results.
Surgical Options
Surgery is considered for morbid obesity or when other treatments fail. Procedures like gastric bypass or sleeve gastrectomy reduce stomach size. These surgeries limit food intake and change digestion. Surgery requires lifelong lifestyle changes and medical follow-up. It can lead to significant and sustained weight loss.
Monitoring And Managing Bmi
Monitoring and managing BMI is key to understanding obesity and morbid obesity. Tracking changes in BMI helps identify health risks early. It guides decisions on lifestyle and medical care. Proper management can reduce complications and improve quality of life.
Regular Screening
Regular BMI screening is important for early detection. Measuring BMI every few months helps track trends in weight. This allows timely action to prevent obesity from worsening. Healthcare providers use BMI results to suggest diet and exercise changes. Screening is simple, fast, and non-invasive.
Role Of Waist Circumference
Waist circumference measures fat around the abdomen. Abdominal fat links closely to heart disease and diabetes risk. Combining waist size with BMI gives a clearer health picture. A large waist with a normal BMI still signals risk. Waist measurement is easy and adds valuable health information.
Tools Beyond Bmi
BMI alone does not show muscle versus fat. Body fat percentage tests offer more detail on body composition. Skinfold calipers and bioelectrical impedance are common methods. Other tools like waist-to-hip ratio also assess fat distribution. Using multiple tools improves monitoring and management strategies.
Coding And Diagnosis Challenges
Accurate coding and diagnosis of obesity and morbid obesity remain complex tasks for healthcare providers. Differentiating between obesity classes using BMI requires careful documentation and precise coding. These challenges impact treatment plans, insurance claims, and patient outcomes. Understanding coding nuances and insurance rules is vital to ensure proper care and reimbursement.
Medical Coding For Obesity
Medical coding for obesity involves selecting the correct ICD codes based on BMI ranges. Obesity codes differ from morbid obesity codes, reflecting severity levels. Coders must verify the BMI documentation in the medical record to assign accurate codes. Inaccurate coding can delay treatment or affect insurance coverage. Clear distinction between obesity classes helps providers capture the true health status.
Insurance Considerations
Insurance companies often require specific documentation for morbid obesity claims. Coverage for treatments like surgery depends on meeting BMI thresholds. Claims may be denied if coding does not match clinical notes. Insurers also look for evidence of obesity-related conditions, such as diabetes or hypertension. Proper diagnosis coding supports approval of treatments and reduces claim rejections.
Documentation Best Practices
Providers should record exact BMI values and obesity class in patient charts. Notes must include relevant symptoms, comorbidities, and treatment plans. Using standardized language improves clarity for coders and insurers. Regular updates to documentation ensure it reflects the patient’s current health status. Thorough and consistent records prevent errors and support better patient care.

Credit: www.foreseemed.com
Conclusion
Understanding the difference between obesity and morbid obesity is key. BMI helps classify weight and potential health risks. Obesity ranges from moderate to severe, with morbid obesity being the highest risk. Both conditions affect health but need different levels of care.
Keeping track of BMI supports better health choices. Small steps can make a big difference in managing weight. Stay informed and seek help if needed. Your health matters most.

