Are you concerned about your weight and wondering what steps you should take to understand your health better? Knowing exactly what obesity evaluation means can be the key to unlocking a healthier you.
Obesity evaluation isn’t just about stepping on a scale—it’s a detailed process that helps uncover the root causes of weight gain and the risks it may bring to your body. By understanding this evaluation, you can take control of your health with clarity and confidence.
Keep reading to discover how healthcare professionals assess obesity, the tests involved, and why this knowledge matters for your well-being. Your journey to a healthier life starts here.
Obesity Basics
Obesity is a condition with excess body fat that affects health. It increases risks of diseases like diabetes and heart problems. Understanding obesity starts with knowing how it is measured and classified. This helps in planning the right treatment and care.
Doctors use different methods to evaluate obesity beyond just weight. These tests give a clearer picture of body fat and its impact on health. Knowing the type of obesity also guides the best ways to manage it.
Body Mass Index And Beyond
Body Mass Index (BMI) is a common tool to check obesity. It uses weight and height to estimate body fat. A BMI over 30 usually means obesity. But BMI does not show fat distribution or muscle mass.
Other tests include waist size and body fat percentage. Waist circumference measures belly fat, which is risky for health. Body fat tests show fat compared to muscle. These give a better idea of obesity’s effects.
Types Of Obesity
Obesity can be different in how fat is stored in the body. There are mainly two types: android and gynoid. Android obesity stores fat around the belly and organs. It has higher health risks like heart disease.
Gynoid obesity stores fat around hips and thighs. It is less harmful but still affects mobility. Identifying obesity type helps doctors choose the right treatment. It also helps people understand their own health better.
Assessment Methods
Assessing obesity involves several methods to understand body fat and health risks. These methods help doctors decide the best treatment. Accurate evaluation is key to managing obesity effectively. Measurement techniques vary from simple tools to advanced tests. Each method gives important information about body weight and fat distribution.
Physical Measurements
Physical measurements are the first step in obesity evaluation. Common tools include weighing scales and measuring tapes. Body Mass Index (BMI) is calculated using weight and height. BMI helps classify weight status from underweight to obesity. Waist circumference measures fat around the abdomen. High waist size often indicates higher health risks. Waist-to-hip ratio compares waist size to hips. These simple tests are quick and inexpensive. They provide a basic understanding of body fat levels.
Body Composition Tests
Body composition tests give detailed information about fat and muscle. These tests separate fat mass from lean body mass. Bioelectrical impedance analysis (BIA) sends a small electric current through the body. It estimates body fat percentage based on resistance. Dual-energy X-ray absorptiometry (DEXA) scans measure bone, fat, and muscle. Skinfold calipers pinch the skin to estimate fat thickness. These tests help identify hidden fat not seen in physical measurements. They provide a clearer picture of obesity and health risks.
Laboratory Tests
Laboratory tests play a vital role in evaluating obesity. They help identify health risks linked to excess weight. These tests provide insights into metabolism, organ function, and nutritional status. Doctors use this data to plan effective treatments and monitor progress.
Blood Lipid Profile
The blood lipid profile measures fats in the blood. It checks cholesterol types like HDL and LDL. Triglycerides are also measured. High levels can increase heart disease risk. Obesity often raises these fat levels. This test guides diet and medication choices.
Thyroid And Metabolic Panels
Thyroid tests check hormone levels affecting weight. Low thyroid function can cause weight gain. Metabolic panels assess blood sugar and insulin. These tests detect diabetes or prediabetes. Early detection helps manage obesity-related conditions.
Liver And Kidney Function
These tests evaluate how well liver and kidneys work. Obesity can cause fatty liver disease and kidney strain. Liver enzymes and kidney filtration rates are checked. Results show if organs are damaged or stressed. This information shapes treatment plans.
Vitamin And Blood Count Checks
Vitamin levels, like vitamin D, are tested. Deficiencies are common in people with obesity. A complete blood count checks for anemia and infections. These tests ensure the body has enough nutrients. They support overall health during weight loss.

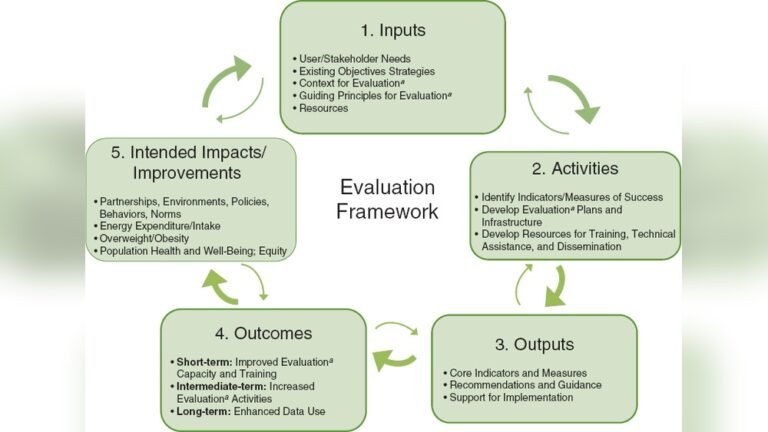
Credit: nap.nationalacademies.org
Diagnostic Imaging
Diagnostic imaging plays a key role in obesity evaluation. It helps doctors see inside the body. This allows them to understand fat distribution and related health risks. Imaging tests provide detailed pictures of organs and tissues. These images guide treatment plans and monitor progress. Different types of imaging tests serve different purposes in obesity assessment.
Mri And Ct Scans
MRI (Magnetic Resonance Imaging) and CT (Computed Tomography) scans provide clear images of body fat. They show the amount and location of fat around organs. This is important because visceral fat increases health risks. These scans also detect fat in muscles and under the skin. They help identify any damage to organs caused by obesity. MRI uses magnetic fields and radio waves. CT uses X-rays to create cross-sectional images. Both are safe and painless procedures.
Electrocardiogram (ecg)
An Electrocardiogram (ECG) measures the heart’s electrical activity. Obesity increases the risk of heart problems. ECG helps detect irregular heartbeats or other heart issues early. It is a simple and quick test. Small electrodes are placed on the skin to record heart signals. This test is important for assessing heart health in obese patients. It guides doctors in preventing serious heart conditions.
Metabolic Phenotypes
Metabolic phenotypes explain why people gain weight differently. These types show how body signals affect hunger and energy use. Understanding these helps tailor obesity evaluation and treatment. Each phenotype has unique traits influencing weight management.
Hungry Brain
The hungry brain phenotype means the brain signals constant hunger. People feel hungry even after eating enough. This leads to overeating and weight gain. The brain’s reward system craves food, especially sugary or fatty items. Managing this type focuses on controlling cravings and improving brain responses.
Hungry Gut
Hungry gut refers to signals from the stomach causing hunger. The stomach empties quickly, sending hunger messages to the brain. This makes people feel hungry soon after meals. It can cause frequent eating and weight gain. Treatments aim to slow digestion and increase fullness.
Emotional Hunger
Emotional hunger comes from feelings, not real hunger. Stress, sadness, or boredom trigger eating urges. Food becomes a way to cope with emotions. This can lead to unhealthy eating habits and obesity. Therapy and stress management are key to this phenotype.
Slow Burn
Slow burn means a low metabolic rate. The body burns fewer calories at rest. This makes it easier to gain weight and harder to lose it. People with slow burn need to focus on increasing activity and boosting metabolism. Proper diet and exercise help manage this type.

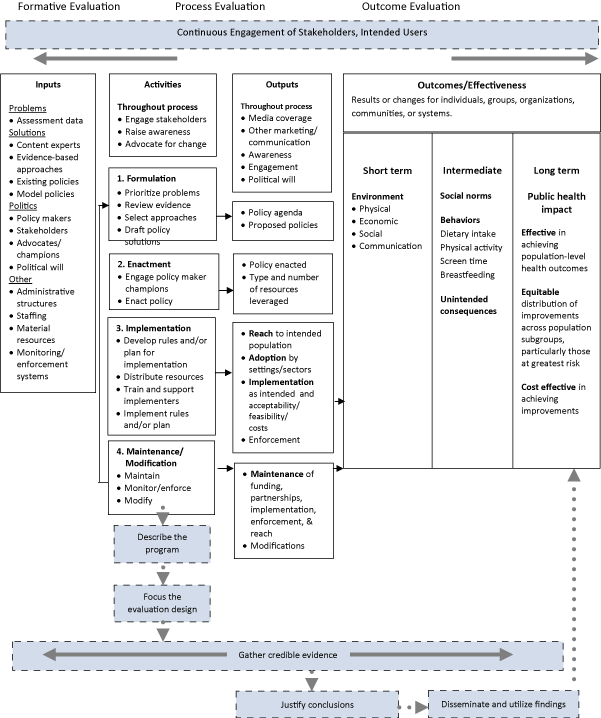
Credit: www.researchgate.net
Risk Factors And Causes
Understanding the risk factors and causes of obesity helps in accurate evaluation. Various elements contribute to excessive weight gain. These elements can be genetic, lifestyle-related, or hormonal. Identifying these factors guides proper treatment and prevention efforts.
Genetic Influences
Genes play a key role in obesity risk. Some people inherit genes that affect appetite and fat storage. These genes can make weight control harder. Family history often reveals patterns of obesity. Genetic factors may also influence metabolism speed.
Lifestyle And Environment
Daily habits impact weight significantly. Poor diet choices, such as high calorie and processed foods, increase obesity risk. Lack of physical activity also leads to weight gain. Environmental factors like easy access to fast food affect lifestyle. Stress and sleep problems can worsen unhealthy habits.
Hormonal Factors
Hormones regulate hunger and fat storage. Imbalances in hormones like insulin and cortisol can cause weight gain. Thyroid problems may slow metabolism and increase fat. Hormonal changes during pregnancy or menopause also affect weight. Understanding these helps in targeted obesity evaluation.
Clinical Evaluation
Clinical evaluation is a key step in assessing obesity. It helps doctors understand the causes and effects of excess weight. This evaluation guides treatment plans and tracks progress. A thorough clinical evaluation involves several important parts.
Medical History Review
The doctor asks about your weight changes over time. Questions cover diet, physical activity, and lifestyle habits. Family history of obesity or related diseases is important. Any previous weight loss attempts and their results are noted. This information reveals patterns and risk factors.
Physical Examination
The doctor measures your height, weight, and waist size. Body mass index (BMI) is calculated to classify obesity level. Blood pressure and heart rate are checked. The exam looks for signs like fat distribution and skin changes. This helps identify health risks linked to obesity.
Identifying Comorbidities
Obesity often comes with other health problems. The doctor checks for diabetes, high blood pressure, and heart disease. Sleep apnea and joint pain are also common issues. Early detection of these conditions improves treatment success. Managing comorbidities is part of obesity care.
Credit: www.cdc.gov
Personalized Treatment Insights
Personalized treatment insights form the heart of effective obesity evaluation. Each person’s body reacts differently to weight gain and loss. Understanding these differences helps doctors create treatment plans that fit individual needs.
Obesity is not the same for everyone. It varies by causes, risks, and how the body stores fat. Personalized insights ensure that treatments target the root causes. This approach improves results and supports long-term health.
Tailoring Approaches By Phenotype
Phenotype means the observable traits of the body. These include fat distribution, metabolism, and appetite. Identifying a person’s phenotype allows doctors to customize treatments. For example, some may have more abdominal fat, needing specific diet and exercise plans. Others may have hormonal imbalances that require different care. Tailoring by phenotype makes treatment precise and effective.
Role Of Surgery And Medication
Surgery can be an option for certain obesity types. Procedures like gastric bypass or sleeve gastrectomy reduce stomach size. This limits food intake and helps with weight loss. Medication also plays a role. Some drugs reduce appetite or block fat absorption. Doctors decide on surgery or medication based on the patient’s health and phenotype. Combining these with lifestyle changes often yields the best outcomes.
Lifestyle Modifications
Lifestyle changes remain essential in obesity treatment. These include diet, physical activity, and behavior therapy. Personalized plans focus on habits that fit daily life and preferences. Small, consistent changes often lead to lasting success. Support from healthcare providers helps maintain motivation and track progress. Lifestyle modifications complement medical treatments and surgery, creating a balanced approach to weight management.
Conclusion
Obesity evaluation helps understand weight and health risks clearly. It uses simple tests like blood work and body measurements. These tests find causes and guide treatment choices. Early checks can prevent serious health problems later. Knowing your body’s condition supports better lifestyle decisions.
Regular evaluations keep track of progress and adjust plans. Taking obesity evaluation seriously improves overall health and well-being.